|
IQR eCQM Requirements
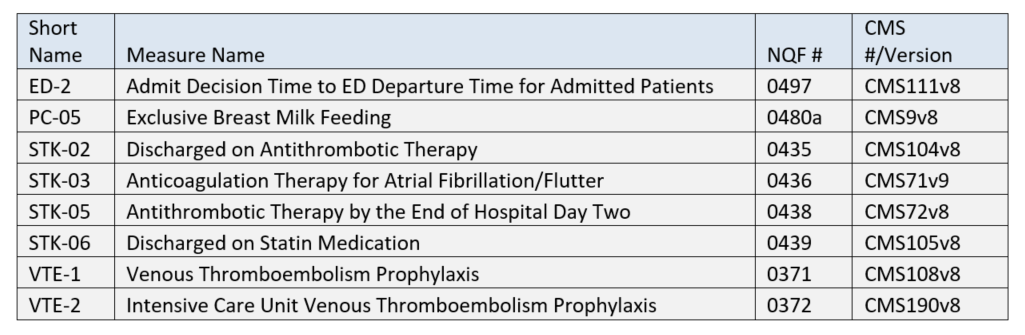
The reporting period continues to be one self-selected quarter of the 2020 calendar year. While you are only required to submit 4 eCQMs, your EHR must be certified for all 8 eCQMs listed above.
More good news! The Quality Net site has been totally re-done. Hands-on users report that the new site is much easier to use than the old. 
Joint Commission
ePC-02 (Cesarean Birth)
Numerator = Nulliparous women with a term, singleton baby in a vertex position delivered by cesarean birth
Denominator = Inpatient hospitalizations for nulliparous patients delivered of a live term singleton newborn >= 37 weeks' gestation
Any DHIT clients interested in reporting ePC-02 should let us know ASAP. |
Wednesday, January 15, 2020
2020 Hospital eCQM Reporting
Friday, January 10, 2020
MIPS/QPP 2020
Now that 2020 is here, how about 20/20 vision to focus on an
outstanding MIPS score? If that’s your
goal, we hope this blog will help! In
case you weren’t paying attention, this is the 3rd year of the
Quality Payment Program (QPP) which spawned the Merit-based Incentive Program (MIPS)
and Advanced Alternative PaymentModels (APMs). The MIPS
2020 Final Rule was published November 1st but maybe you missed
reading due to its 996 page length, the busy holiday season, etc. So here’s our synopsis – for the sake of
brevity, we’ll skip the eligibility and APM criteria and focus on requirements
for those who opt in (voluntarily or kicking and screaming!) for MIPS/QPP.
Overall Scoring and Financial Incentives
- Quality: 45%, Cost 15%, Promoting Interoperability (PI) 25%, Improvement Activities (IA) 15% -- these are all the same as last year and the weighting is unchanged, although CMS is mandated to make all categories 30% by 2022.
- The Performance Threshold increased from 30 points to 45 points. For clinicians, this means you’ll have to score at least 45 points to avoid a penalty. Conversely, the exceptional performance threshold increased from 70 to 85 points.
- Greater financial penalties and rewards – non-participants get dinged 9%. Theoretically, bonuses could also be up to 9% but probably won’t be that high due to budget neutrality requirements.
- Reminder that starting with 2018 (Year 2) data, MIPS scores will be publicly reported on the Physician Compare website.
Quality Performance Category
- Medicare Part B Claims measures: 70% sample of Medicare Part B patients (up from 60%) for the performance period
- QCDR measures, MIPS CQMs, and eCQMs: 70% sample of clinician's or group's patients (up from 60%) across all payers – no “cherry picking” is allowed.
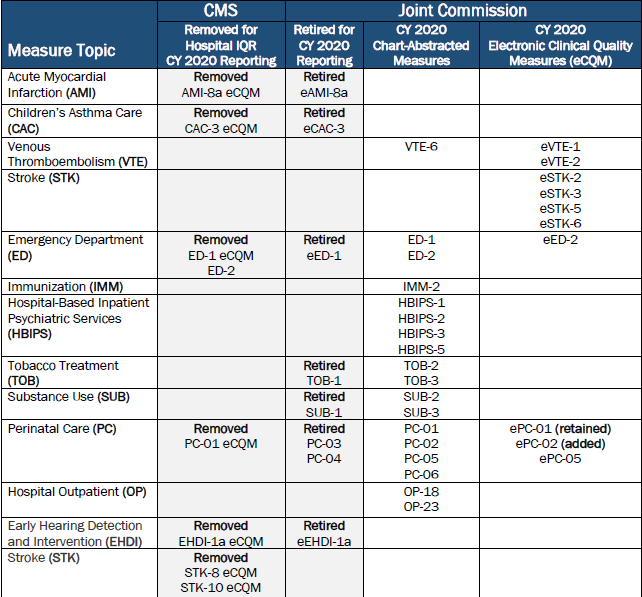
- Driven by the Meaningful Measures initiative, CMS removed 42 measures (quality ID #’s): 046, 51, 68, 91, 109, 131, 160, 165, 166, 179, 192, 223, 255, 262, 271, 325, 328, 329, 330, 343, 345, 346, 347, 352, 353, 361, 362, 371, 372, 388, 403, 407, 411, 417, 428, 442, 446, 449, 454, 456, 467 and 474. Of these, 4 were eCQMs: 160, 192, 371 and 372.
- On page 63214 of the Federal Register Final Rule, there is a table of recommended CQMs by medical specialty. I don’t normally endorse reading the Federal Register but this is a valuable resource. The following specialty areas were added for 2020:
o
Audiology
o
Clinical Social Work
o
Chiropractic Medicine
o
Endocrinology
o
Nutrition/Dietician
o
Pulmonology
o
Speech Language Pathology
Improvement Activities Performance Category
- There are 2 new IAs, 7 modified IAs and 15 that were removed.
- Page 63514 of the Federal Register has a table of all 2020 IAs.
- For groups, the threshold re. number of clinicians for an IA has increased from just 1 to at least 50% of the group for any continuous 90-day period.
Promoting Interoperability Performance Category
- The optional Query of PDMP measure will require a Yes/No response instead of a numerator/denominator.
- The optional Query of PDMP measure has been removed.
Cost Performance Category
- There are 10 new episode-based measures:
Measure
|
Episode Measure Type
|
Acute Kidney
Injury Requiring New Inpatient Dialysis
|
Procedural
|
Elective Primary
Hip Arthroplasty
|
Procedural
|
Femoral or
Inguinal Hernia Repair
|
Procedural
|
Hemodialysis Access
Creation
|
Procedural
|
Inpatient Chronic
Obstructive Pulmonary Disease (COPD) Exacerbation
|
Acute inpatient medical condition
|
Lower Gastrointestinal Hemorrhage (applies to
groups only)
|
Acute inpatient
medical condition
|
Lumbar Spine
Fusion for Degenerative Disease, 1-3 Levels
|
Procedural
|
Lumpectomy Partial Mastectomy, Simple Mastectomy
|
Procedural
|
Non-Emergent Coronary Artery Bypass Graft (CABG)
|
Procedural
|
Renal or Ureteral Stone Surgical Treatment
|
Procedural
|
To Summarize: CMS has once again raised the
bar and the financial stakes, so we recommend starting your MIPS/QPP planning
ASAP and monitoring scores regularly throughout the reporting year. Our Dynamic Registry platform has great tools
for this and is available with or without contracting for our services as a QPP Qualified Registry.
Subscribe to:
Posts (Atom)



